A question heard frequently in private practice is how do we stay on top of paperwork when our passion is engaging the client in doing meaningful work? What if clinical documentation supports them in getting additional resources such as disability or explores reunification with their children? When working with individuals or families involved in the Department of Human Services (DHS), probation, diversion, or other entities evaluating your client, the documentation you keep takes on an additional level of importance in capturing the client’s progress. So how does one balance recording the content of the session consistently while protecting client confidentiality? Balancing requirements for documentation with client privacy is an art form that requires consistency and practice.
Construction of Case Notes
Depending on your preference for hand written, typed, or electronic notes, your content and formatting of those notes could be dictated by private or state assistance insurance panels in order to process claims and receive payment for services rendered. With this in mind, most insurance panels require the following to be identified in each note:
- Full name of client and insurance ID
- Date of service
- Time of Service
- Duration of Service
- CPT Code that indicates individual therapy, family therapy, case management, etc.
- Overview of therapeutic interventions utilized in the session
- Progress towards identified treatment goals
- Current mental health diagnosis
- Client presentation in session
- Next scheduled appointment
By formatting your notes in a similar fashion, you can streamline any documentation needs from secondary parties desiring collaboration. Don’t forget a signed Release of Information from your client to facilitate collaboration!
Consistency in Content
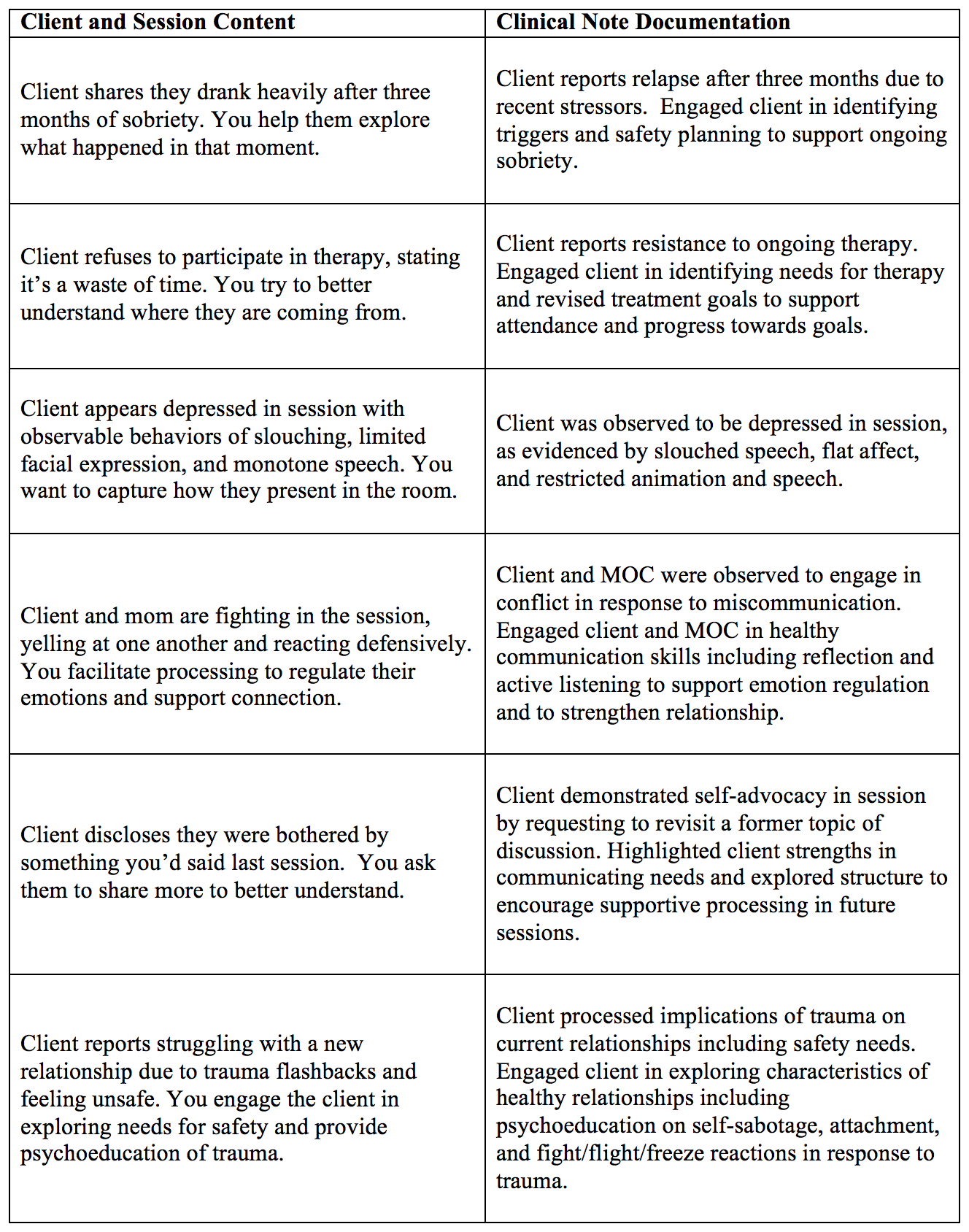
Formatting not only provides the outline of a universal progress note, it can support consistency that will reduce the time spent on notes each week. Many therapists report frustration that their notes are behind schedule due to wanting to dedicate their time and energy to the client work. By utilizing a template for notes, it will become easier and more efficient to complete notes in a timely manner, especially in utilizing clinical language. When struggling with how to write clinical language that captures the professional interventions present in each session, it can be helpful to have some go-to phrases that indicate progress without providing too much detail. Here are some examples of common content and professional language that could be helpful in writing clinical notes:
Confidentiality for Clients
In addition to clinical documentation supporting professional record keeping in line with ethical requirements, another component it can support is client confidentiality. It can feel like a fine line providing adequate written evidence of professional interventions without violating client privacy.
One strategy to ask yourself is, “would my client feel uncomfortable with my notes being seen in court or by others?” If the answer is yes, you may want to re-evaluate how you write your notes to support clear, concise interventions that would not put confidentiality at risk. Below are some documentation tips to consider in supporting client privacy:
- Keep client direct quotes to a minimum. They are best included when capturing safety concerns. Client reported “I want to die” leading to assessment and safety planning in session.
- Avoid emotion-driven language without evidence such as, client was happy/sad/angry in session.
- Support ownership of statements such as, this writer observed or client reports when documenting statements or content of a session.
- Keep language neutral. It is best to avoid a positive or negative tone in notes to prevent accusations of bias or alignment that would put professionalism in question.
It is recommended you seek consultation or supervision to further explore your documentation needs. Your professional organizations can provide ethical guidelines whereas insurance panel websites offer Providers valuable templates for clinical documentation that meet audit standards. With luck, you will perfect your clinical writing to maximize time in therapeutic interventions while remaining compliant with documentation needs to best serve your clients and your practice.