Working with children in a therapeutic setting can be very rewarding and can prevent further problems with mental health and behavioral issues down the road. Most therapists that choose to work with kids are comfortable sitting on the floor, engage easily with children and are comfortable setting boundaries around safety in the play therapy room. Engaging and setting boundaries with parents can be an entirely different ball game. And unfortunately, establishing a supportive and collaborative relationship where firm boundaries are set in place with the caregivers may be as important as your relationship with the child in order to facilitate positive change. If you are in a private practice setting, there is another layer of importance to engaging parents. Your income depends on you maintaining a caseload of happy parents, as well as children who are improving.
You and the child can do great work in the play therapy room, improving self-regulation, verbalization of feelings, and allowing for an unconditional, child-centered relationship to allow the child to process the most difficult situations and it can be completely unraveled once the child returns home for the week if they are not set up for success at home. Taking two steps forward and then one or two steps back each and every week can be disheartening for the child, caregivers and us as therapists. This is why it is paramount to engage your parents to be a helpful partner in this process. So what do you do if a caregiver to one of your kids is unwilling to make changes or is so stuck in their trauma or emotions regarding a divorce that they are not acting as your partner in the therapeutic process? What if all they are looking for is for you to provide testimony in family court that supports their beliefs about the family situation? How can we as therapists, advocates, and potentially the only objective person in the situation bring about positive change in the lives of these children?
Thorough Preparation is Key
In my twelve years of experience working with children and teens in a therapeutic setting, I have learned that the most important aspect of creating an appropriate and collaborative relationship with caregivers where boundaries are respected and maintained starts before your first interaction. It is important to have a clear understanding of your scope of practice, what you are or are not willing to provide for families, the laws around decision-making and custody in your state, the laws of age to consent to mental health services in your state, and the policies and procedures for your practice or the agency you work for before you call that parent back to set up an initial session. If you are not clear in your own mind of these things, you are more likely to set up a relationship where you have to back track or get stuck in a situation later on. For example, if a parent calls to get their child in for counseling with you and you do not inquire if there are any issues with custody or if any other parent shares decision making responsibilities in that initial phone call, you do not know if you are able to see that child. You are putting yourself and credentials at risk by not asking the right questions during that initial phone call. If there is shared decision making responsibilities, then you can educate the parent about the laws of your state and request the appropriate court documents to show any current orders in place. Along with having clarification in your own mind about these issues, you also have to have them represented in your initial paperwork so that you have a way to discuss all of these issues with the caregiver. It is important to have fees, policies around communication, policies around providing court summaries or court testimony (including fees), and the rights of the child in your disclosure and consent. This way, the parent has the information upfront and has signed in agreement that this is in fact how you will be running the show. And then, it’s up to you to put it into practice.
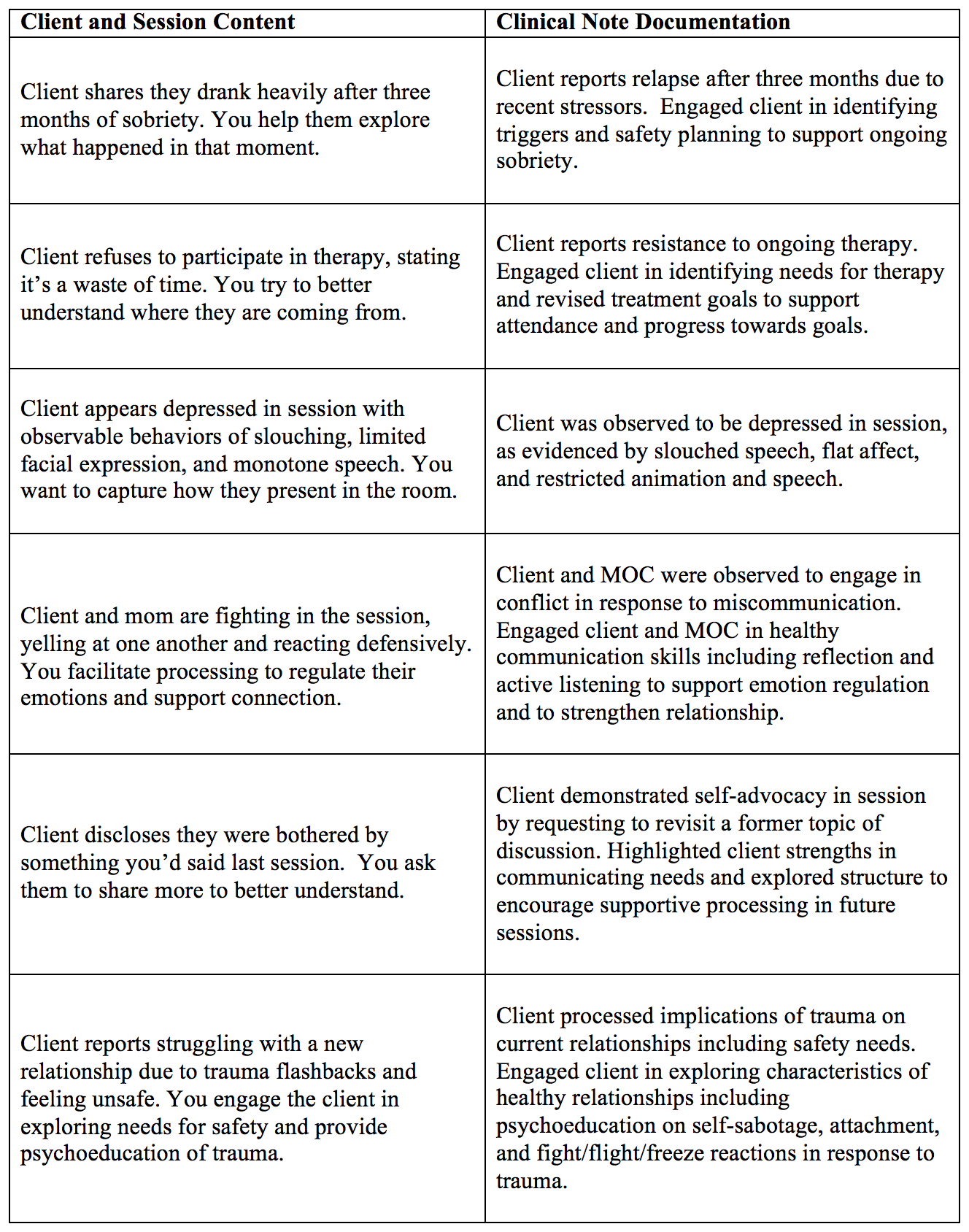
Documentation
How do you engage parents and maintain this engagement even when they do not agree with you or have a specific agenda they expect from you? Even if you have started off the relationship with strong boundaries, many parents are still so stuck in their own stuff that they will test your boundaries. Working with these parents is frustrating to say the least. You see the positive changes that the child is making in session and know that they could improve significantly more if the parent followed your recommendations or if they weren’t so focused on making the other parent look bad. Two things…continue making the recommendations that will benefit your kiddo, continue being their advocate, and document, document, document. Unfortunately in our very litigious culture, you will need to have good documentation of what was recommended and why, as well as if caregivers followed through with the recommendations. If you are ever grieved, you have everything you need documented to show appropriate care. It can also be helpful for you to keep track of specific recommendations that were attempted, versus the ones that are not. This can inform the recommendations you make in the future.
Communication Strategies
Another area that I have consulted with many child therapists on is how to manage parents going through a conflictual divorce, specifically so that they are not being triangulated into the relationship and can continue to focus on the best interest of the child. Again, the importance of having the discussions around your policies is paramount. I typically have two separate intake sessions if I have the chance, so that I can go through the information thoroughly and so that there is not the perception that I have a better relationship with one parent or the other. I also recommend that most correspondence is done through email (if both parties agree to using email for therapeutic information after understanding the possible issues with confidentiality), and that all correspondence is sent to both parties. This way there is less possibility for he-said-she-said concerns about what your recommendations are. I stick to this policy unless there is a significant safety concern or if there is a no-contact or restraining order in place between parents. I ask that caregivers put the other parent on any emails sent directly to me, however this boundary is always broken. I have already let parents know that anything I send out will go to both parents, so if they need a reply, it will get sent to both parents. If it does not need a reply, I keep the emails as documentation, reply that it is important that all emails go to both parties unless there is a safety issue, and use it as data for my own conceptualization of the case.
There are many other logistical tips that could be provided to working with difficult parents. The tip that I have found the most helpful in maintaining positive relationships with parents that I have to continually challenge or set firmer boundaries is to remember that they are human beings with their own histories. I believe that most parents are doing the best they can with what they’ve got at the time. This may not be very good at all, but there are reasons for their behavior. Remembering this allows me to be personable with them even when extremely frustrated. And remembering that you may be the only safe person in your child’s world at this moment, provides enough incentive to do the hard work of managing their caregivers.
Guest post written by Sybil Cummin, MA, LPC, ACS
Sybil Cummin, MA, LPC, ACS is the owner and clinical director of Arvada Therapy Solutions, PLLC. Sybil's specialties include working with children, teens and families dealing with family trauma including conflictual divorce, child abuse and neglect, sexual abuse, and domestic violence. As an Approved Clinical Supervisor, she also supervises Master's level interns and clinicians working towards licensure, as well as providing business consultation to therapists embarking on the world of private practice.